j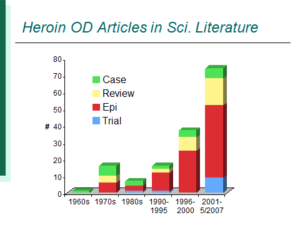 This chart was produced in 2007 to demonstrate the increase in overdose literature in the late 1990s and early 2000s – a trend that has continued. Twenty years ago there would have been 1 article for this post every 3-4 months, which may have been okay since you would have received it by actual post.
This chart was produced in 2007 to demonstrate the increase in overdose literature in the late 1990s and early 2000s – a trend that has continued. Twenty years ago there would have been 1 article for this post every 3-4 months, which may have been okay since you would have received it by actual post.
Read on for a month of 8 papers laden with epidemiology…
Garfein RS, Rondinelli A,Barnes RF, Cuevas J, Metzner M, Velasquez M, Rodriguez D, Reilly M, Xing J,Teshale EH.
J Urban Health. 2012 Jul 6.[Epub ahead of print]
Comment: Focusing on the overdose component of the manuscript: Dr Garfein and colleagues found a relatively low rate of lifetime overdose in this cohort of 18-40 year olds of 28.1% (an analysis of these data with overdose as the outcome is clearly warranted). Most notably, they found an independent association of history of overdose with HCV infection.
This is consistent with other recent data suggesting an association between overdose and other drug-related risk behaviors such as syringe sharing. A poster this month at the International AIDS Conference shows that those who administer naloxone at their most recent witnessed overdose are less likely to share syringes than those who didn’t administer naloxone. Moreover, the reductions in overdose we have seen in regions with well-funded naloxone distribution programs have been far more impressive than mathematical modeling would suggest. All together, these data force me to wonder if naloxone distribution has an effect well in excess of its ability to reverse an overdose.
2) Estimating the prevalence of illicit opioid use in New York City using multiple data sources.
McNeely J, Gourevitch MN, Paone D, Shah S, Wright S, Heller D.
BMC Public Health. 2012 Jun 18;12(1):443. [Epub ahead of print]
Comment: An excellent team of authors has attempted the perhaps impossible task of estimating the number of opioid users in New York City – a task that was hard enough with heroin alone. The results seem consistent enough to what would be predicted by large-scale epidemiologic studies to be of substantial use in future. I’ve asked for additional thoughts on this approach and will post comments when they come.
3) Low-Frequency Heroin Injection among Out-of-Treatment, Street-Recruited Injection Drug Users.
Harris JL, Lorvick J, Wenger L, Wilkins T, Iguchi MY, Bourgois P, Kral AH.
J Urban Health. 2012 Jun 12. [Epub ahead of print]
Comment: Among “low frequency” heroin users (who used 1-10 times in the past 30 days) 7.0% had overdosed in the past year. Among “high frequency” heroin users, 14.8% had overdosed in the past year. So infrequent heroin injectors overdose less in this sample. The low frequency injectors were marginally older, which may partially explain less overdose (that is, users who survive to older ages are less likely to overdose in a given year), yet I am still somewhat surprised by this result as I would presume low frequency injectors would have low or inconsistent opioid tolerance that might raise their risk of overdose. At this time, we clearly can’t consider bouts of abstinence as a behavioral risk factor for overdose.
4) Vital signs: risk for overdose from methadone used for pain relief – United States, 1999-2010.
Centers for Disease Controland Prevention (CDC).
MMWR Morb Mortal Wkly Rep.2012 Jul 6;61:493-7.
Comment: Methadone has been the likely culprit for a large portion of prescription opioid deaths in the U.S. in the past 8-9 years. This likely occurred for a couple of reasons. First, extended release oxycodone was associated with a surge in opioid overdose deaths 10-12 years ago, so switching to methadone as the long-acting opioid seemed reasonable at the time. Unfortunately, dosing of methadone is complicated, with a non-linear dose-response curve that makes doses over 30mg dangerous for methadone-naive patients.
Gudin J.
J Pain Palliat Care Pharmacother. 2012 Jun;26(2):136-43.
Comment: I don’t have access to this one, but it’s an interesting piece on prescription opioids requirements emerging from the FDA. The Project Lazarus site has more information.
6) Patterns of Prescription Drug Misuse among Young Injection Drug Users.
Lankenau SE, Teti M, Silva K, Bloom JJ, Harocopos A, Treese M.
J Urban Health. 2012 Jun 9. [Epub ahead of print]
Comment: Very interesting qualitative piece on use of prescription opioids by young heroin injectors. One harm reduction strategy noted by study participants was to substitute prescription opioids for heroin when there was an outbreak of heroin overdose deaths in the community.
7) Cheese: An old drug in a new wrapper.
Maxwell JC, Coleman JJ, Feng SY, Goto CS, Tirado CF.
Drug Alcohol Depend. 2012 Jul 3. [Epub ahead of print]
Comment: A mixture of heroin, Benadryl, and APAP (basically tylenol) – this is an intriguing report of the use of “cheese” heroin in Dallas, Texas, with an appropriate attention to overdose. As authors experienced, overdose data are limited and disappointing given the severity of that consequence.
Freise KJ, Newbound GC,Tudan C, Clark TP.
J Vet Pharmacol Ther. 2012Aug;35 Suppl 2:45-51.
Comment: Naloxone reverses this long-acting fentanyl solution in beagles. I’m not clear from this what the dose requirements are for naloxone in this situation.
That bullet 7 there is a bit compelling! Was that verified at least? It makes me cringe going for a Three trees dental services just to get my Tylenol prescription. I hope that can be verified.